An efficient revenue cycle yields more than just back-end benefits - it can even improve the patient's financial experience.
A focus on straight-through-processing (STP) that leverages technology like AI and machine learning helps create a more accurate revenue cycle. This drives additional billing events and corrects erroneous data fields. Perhaps most importantly, when utilizing AI and machine learning to electronify paper and PDF-originated EOBs/EOPs, the data extracted is able to be imported to multiple systems, including denial analytics platforms where data was previously unavailable or extremely difficult to import. This enables providers and RCM servicers to find patterns in denials to refine decision-making and build a feedback loop that results in continuous revenue cycle improvement.
Typically electronification focuses on providers, clearinghouses, and payers, but patients also stand to benefit from data that enriches the denials process.
How Denials Issues Impact Patients
Patients find bills confusing and frustrating.
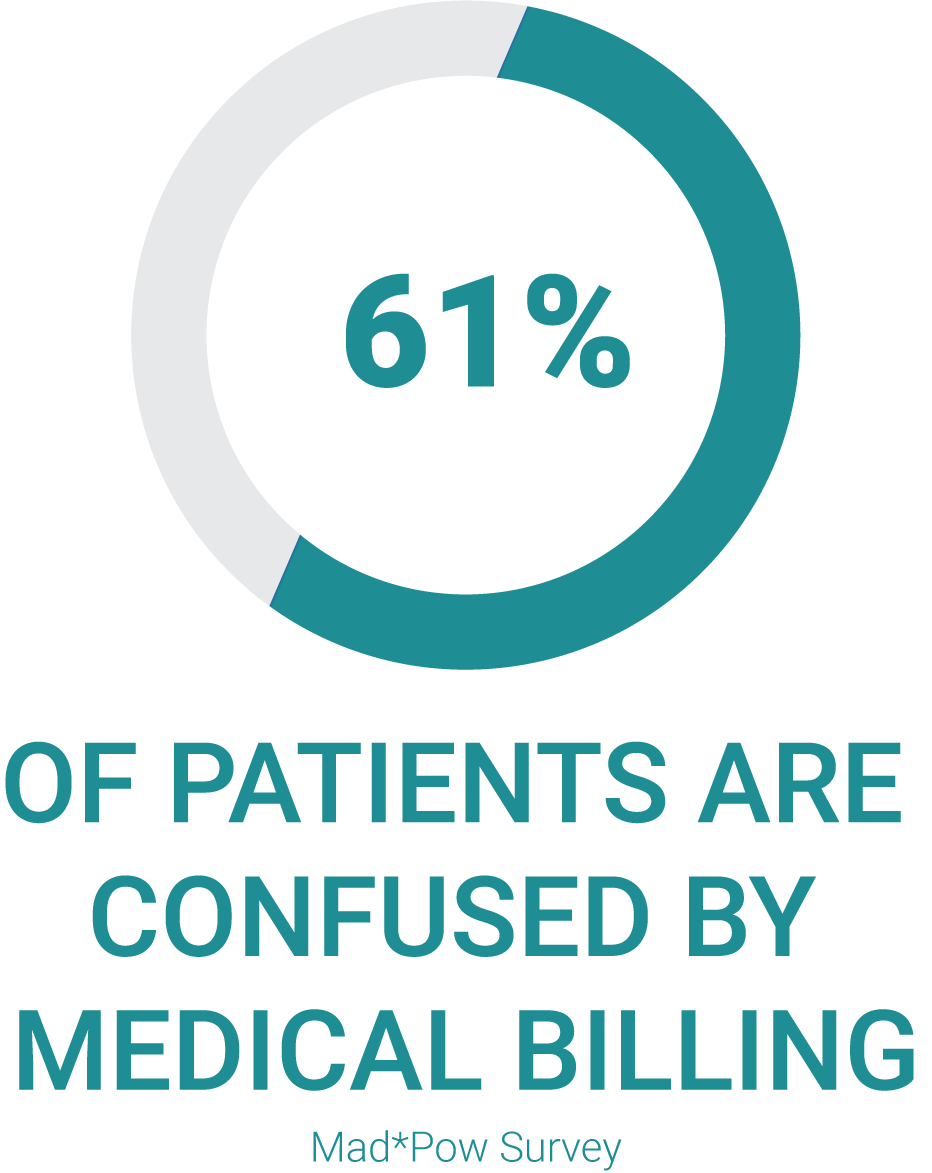
A Mad*Pow survey found that 61% of patients are confused by medical bills. Over half of their respondents blamed the relationship between bills from the provider and insurance company statements as the cause of frustration. Over 49% said they were unsure if the total owed was correct.
How much worse is that experience when patients are caught up in the back-and-forth process of billing disputes, denials, appeals, and corrections?
For example, if the wrong ICD code is used, a claim might be denied and patients might be billed for services that were incorrect or they did not receive. This could result in a patient being billed more and the payer paying less than their contractual obligation.
By focusing on accuracy improvements, providers and revenue cycle servicers have an opportunity to decrease incorrect coding practices. This helps reduce the risk that patients are billed for the services they’re not responsible for, or the chance they find out months down the road that their responsibility is higher than they were originally told. Additionally, a denials analytics platform that incorporates electronic and paper EOBs/EOPs allows for providers and RCM servicers to see trends and take proactive and corrective measures to minimize common errors that affect patient billing.
The Trickle-Down Impact of STP
Avoiding denials and getting claims right on the first round of billing positively impacts the patient financial experience. That goal is reached by focusing on accuracy on the back-end and applying technology that learns continually, finds and corrects errors, and feeds back into a more accurate, straight-through revenue cycle.
Revenue cycle management is only going to become more complicated over time. PDF and paper volumes are expected to grow and today, patients stand as the third-largest payer behind Medicare and Medicaid, meaning that they will feel the impact of any back-end issues that do crop up. Both providers and payers will need to focus on analyzing denial trends (incorporating both electronic and paper/pdf-originated claims) like non-covered charges, missing claims information, and precertification and authorization issues to perform root cause analysis and correct issues going forward.
It’s time to take a strategic orientation toward your denials management and leverage data aggregation that benefits every stakeholder in the revenue cycle.
Watch this two-minute video on how a denial analytics platform which incorporates both electronic and paper/PDF-originated remits can support this environment.
