Access Denial Intelligence
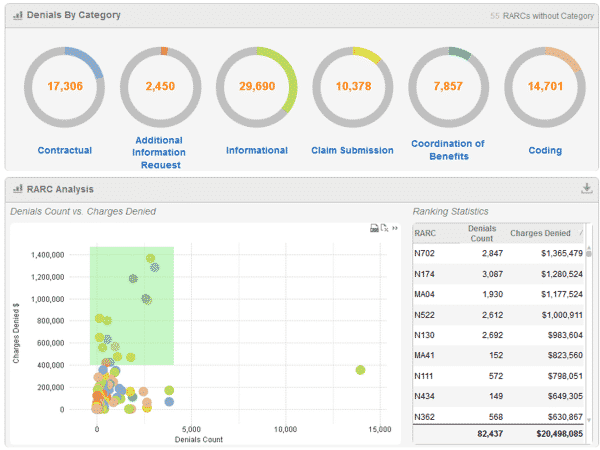
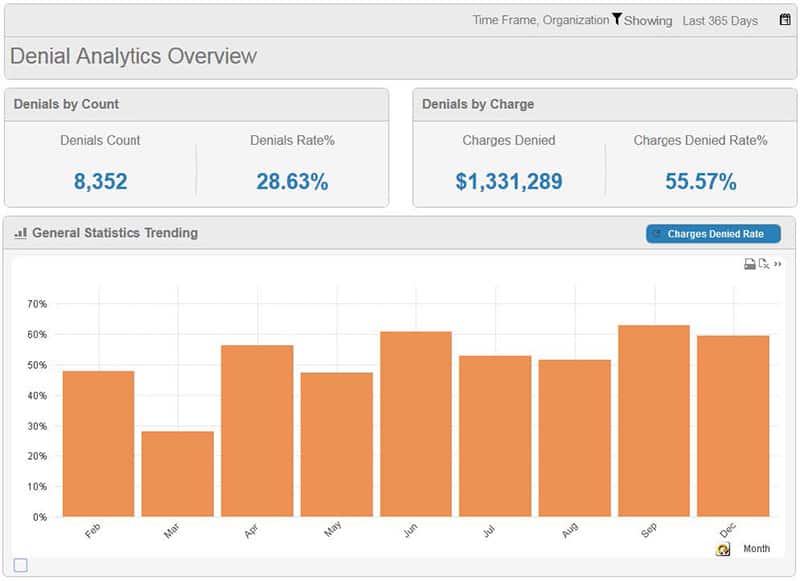
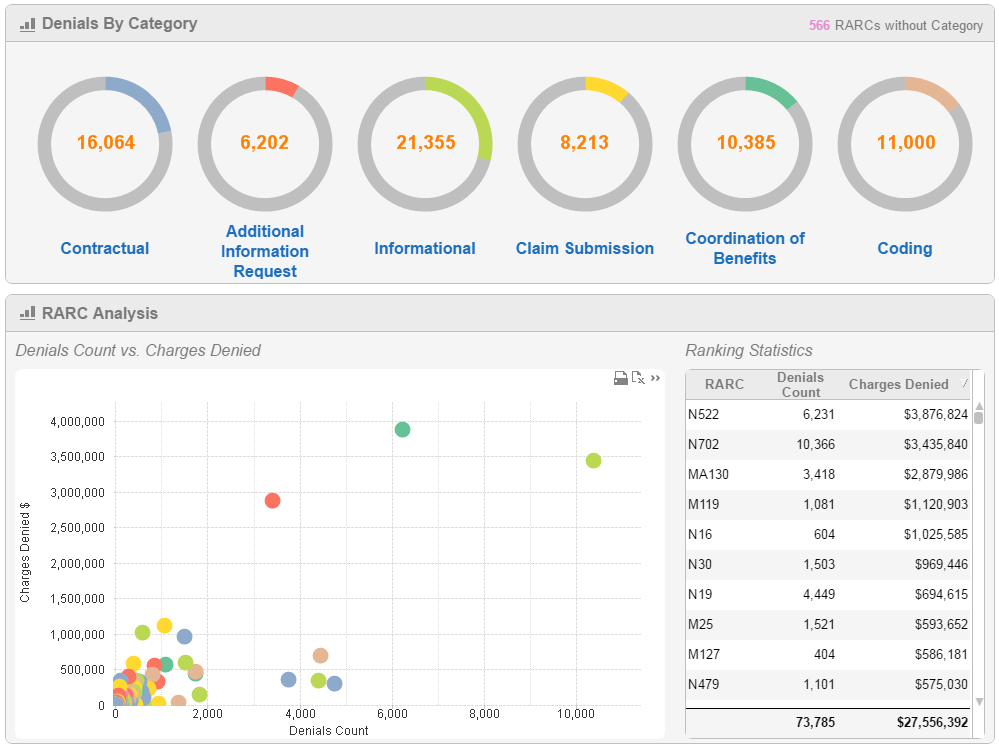
Access Denial Intelligence is the newest addition to the OrboAccess suite. The system analyzes and identifies denied claim trends and improves work processes as a decision support resource.
Built on the framework and technology of business intelligence, reporting views can be “sliced and diced” from a variety of interrelated data sources including; EDI 837 claims, EDI 835 ERA, EOB/EOP, ACH, and checks. By incorporating both clinical and revenue cycle data into insightful metrics, management can identify and prioritize problematic trends in denied claims. The result is to maximize the recovery of revenue on denied claims, reduce leakage, and shorten accounts receivables.
The system offers a highly intuitive user experience designed for use by multiple levels of management and users across the healthcare provider. C-level and revenue cycle management can use the system as a benchmark for success, monitor key performance indicators (KPIs) and create direction for proactive denial correction. The system also delivers predefined schedule reports.
Join OrboNation
Access to critical updates, new industry insights, & thought leaders.
