Healthcare Industry
Becker’s announcement on CMS’ DME prior authorization rule came a while back, but CMS’ stance on prior authorization is likely still causing denial issues for your facility today. The Backstory Just as 2016 was about to round the corner, CMS issued a rule requiring prior authorization before Medicare would reimburse DME that had been found…
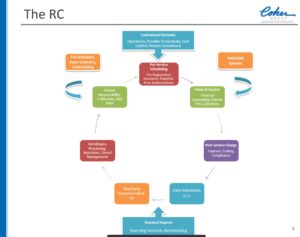
Read MoreWe recommend you buy a Starbucks coffee and set aside an hour to watch the “Coffee With Coker” presentation entitled “Revenue Cycle Turnaround: Rebuilding for an Advanced ROI – A Case Study,” which is archived here. Senior Vice President of Coker Group Jeff Gorke takes us through the components and challenges of building and maintaining…
Read MoreA recent report from Grand View Research reveals a potentially hidden threat to telemedicine programs. We’re all aware that chronic disease is a growing problem around the world, but did you know that the diabetic foot ulcer treatment market alone is valued at over $3.15 billion? Statistics like that mean the results of a report…
Read MoreEHR Intelligence reports on a whopping sixty-two Indiana hospitals being sued in a federal civil lawsuit for allegedly falsifying records and participating in a kickback scheme, primarily by overbilling for the release of patient Electronic Health Records. As reported in The South Bend Tribune: Memorial Hospital of South Bend, Saint Joseph Regional Medical Center in Mishawaka,…
Read MoreEarlier this year, The Huffington Post reported on the largely negative impact Medicare regulations are having on CPAP users and providers. On the provider side specifically, CPAP denials have been known to top denials lists for HME and DME suppliers, meaning that understanding the layers of Medicare’s logic is the first step in understanding how…
Read MoreThe CHANGE HEALTHCARE HEALTHY HOSPITAL REVENUE CYCLE INDEX estimates that out of the $3 trillion in claims that were submitted in 2016, 9 percent ($262 billion in charges) were initially denied. For your average health system, that adds up to as much as 3.3 percent of NPR, dinging them for an average of $4.9 million…
Read MoreBecker’s ASC Review reports that Millennials, or individuals born roughly between 1980 and 2000, now number 73 million in the United States (according to the polling firm Gallup). They are well on pace to soon outnumber Generation X — their immediate predecessors — at all U.S. companies. For review, here’s a timeline (just one of many…
Read MoreIt looks like 2018 is going to be the year of denials and that’s exactly as foreboding as it sounds. Becker’s article based on the Advisory Board’s survey revealed that denials written-off as uncollectable, costs the average 350-bed hospital $3.5 million annually; a whopping 90 percent jump from just six years prior. Compounding this challenge…
Read MoreWe operate in an already complicated reimbursements environment, so anything we can do to minimize the constant threat of denials is going to help the entire revenue cycle. Becker’s Hospital Review produced a helpful webinar discussing strategies to prevent claims denials that can be accessed here. In an article summing up the presentation, Becker’s distills…
Read MoreAn article on the HealthExec website describes a Health Care Payment Learning and Action Network (LAN) report recently released, showing that 43 percent of payments to health systems came from traditional fee-for-service (FFS) payment models in 2016. That’s down from 62 percent the year before. Meanwhile, alternative payment models’ (APMs) share increased from 23 percent to 29 percent. While…
Read More